I was a young psychiatry resident at the University of Pennsylvania Medical School; after two years, I could be seen fleeing from the many different models and innovators, including Professor Aaron Beck, founder of Cognitive Behavior Therapy (CBT).
I was headed, with haste, across campus, to the Philadelphia Child Guidance Clinic (PCGC), where it was purported that Salvador Minuchin was “curing” juvenile diabetes with family therapy. Of course, he was not doing that, but he was mitigating the family stress that exacerbated biological diabetes mellitus. I breathed a sigh of relief as my teachers and supervisors paid attention to the context of an individual and utilized grounded theory. My identity crisis was averted; I was admitted into child psychiatry and I had found my home.
Braulio Montalvo, Jay Haley, and Marianne Walters were my teachers, along with Dr. Minuchin. It was, I imagine, much like Paris was in the twenties for the art world; a time of great creativity. Each episode of supervision was imbued with excitement and respect. I watched as Structural Family Therapy shifted the focus of the problem from the youngsters and artfully anointed the family members as agents of change. It was powerful and beautiful, and just made so much sense. It was an important time in my newly developing career.
This potent model of care demonstrated that anorexia nervosa could be treated quickly and efficiently, with the youngster eating in the first or second therapeutic session. A long way from the traditional treatment, languishing in hospitals with the dreaded nasogastric tube delivering nutrition. So disappointing to know that today, 45 years later, I am often called on to treat these 15 year olds after two to three failed hospitalizations. Tradition has a stranglehold on institutions.
Structural Family Therapy was destined to be the great liberator—it did not happen. Evan Imber-Black describes the “model wars” of the early days where the leaders would travel across the world and proselytize (2014, p. 372). Minuchin, Haley, and Whitaker did it, and so did many others. The followers would sit in awe as Selvini or Bowen or Satir described in detail their work; White and Epston were on the heels with Narrative Therapy. Family therapy was brimming with promise, and it seems model migration required keeping up with the changing styles, not published outcomes.
We were confident that family therapy would become the gold standard psychotherapy. Sadly, we were mistaken. CBT has assumed that position. Peter Fraenkel (2022, p. 23) reports family therapy training went from being a comprehensive paradigm to being just one more alternative modality, like group therapy. He blames the social forces of the market place: managed care and evening hours that led individual models to marginalize the field.
The fatal flaw of these evolving family therapies was the blindness to outcome data; the repackaged newness just seemed to capture all the attention. Understandably, with the paucity of researched outcomes failing to support any model over the next, choosing newness was the default mechanism.
Gold standards be damned. As a psychotherapy field, we are failing, according to Stanford University Professor John Ioannidis. Using both a meta-analysis and randomized controlled trials (RTCs) of psychotherapy and psychopharmacology, Ioannidis et al. (2005) found that the efficacy is limited; no better than waiting lists. The Atlantic stated in a special edition about “Brave Thinkers,” that Ioannidis may be one of the most influential scientists alive (Freedman, 2009). A prodigious researcher with over 2,000 referenced journal articles, he deserves our attention. The most accessed article (three million downloads) in the history of the Public Library of Medicine is Ioannidis’ Why Most Published Research Findings are False (2005).
I don’t think we moved the needle in reducing suicide, reducing hospitalizations, improving recovery for the tens of millions of people who have mental illness.
Another revered researcher, Dr. Tom Insel, when he was leaving the directorship of the National Institute of Mental Health (NIMH), reflected, “I spent 13 years really pushing on the neuroscience and genetics of mental disorders, and when I look back on that, I realize that while I think I succeeded at getting lots of really cool papers published by cool scientists at fairly large costs—I think $20 billion—I don’t think we moved the needle in reducing suicide, reducing hospitalizations, improving recovery for the tens of millions of people who have mental illness. I hold myself accountable for that” (Rogers, 2017, para. 6). He went to work at Google (and eventually moved to Mindstrong, a company aiming to come up with technologies to diagnose and treat mental disorders).
The researchers tell us that mental healthcare is shockingly disappointing and the costs are astronomical. Ringel and Sturm’s adjusted calculations for inflation estimated that the total cost to the U.S. economy of all childhood emotional and behavioral issues could be as high as US$247 billion per annum (Perou et al., 2013, cited in Leichsenring, Steinert, & Ioannidis, 2019). According to Leichsenring et al. (2019), “The Lancet commission on global mental health and sustainable development estimated a loss of US$16 trillion to the global economy due to mental disorders in the period 2010–2030” (p. 1). These findings are disappointing and not surprising; perhaps a result of the endemic quality deficits.
Some family therapy researchers have tracked and published their outcomes successfully. The Maudsley Model of Family-Based Treatment (Le Grange & Lock, 2005) for anorexia nervosa and two models for the treatment of conduct disordered children are notable for their excellent outcomes. The protocolized Multisystemic Therapy (MST) and Functional Family Therapy (FFT), along with Maudsley, have worldwide utilization. Outside of these few models, family therapy remains increasingly undocumented.
Introducing results-based accountability
In the middle 1990s, government programs were sharing space in the same ‘outcome void.’ States were hemorrhaging money. Mark Friedman, having spent 20 years managing the finances of children’s services for the state of Maryland, developed Results-Based Accountability (RBA; Clear Impact, 2016). After spending so much money, he wanted to answer the question, “Is anyone better off?” His book, Trying Hard is Not Good Enough (Friedman, 2015) has sold 75,000 copies. RBA was a resounding call to action for public services; all 50 states and many countries, including New Zealand, adopted his common-sense framework.
A Medicaid mental health service in Philadelphia for 500,000 insured lives suffered the same problem. As chief medical officer in the 1990s, I directed the clinical care; when I rummaged through the glossy brochures of the non-profit programs on offer, there were no outcome data. I was piloting a plane with no altimeter.
When I relocated to the other side of the world in 2001 with my family, there it was again, another data free zone treating severely troubled adolescents. Having followed RBA’s wide acceptance, I wondered if the framework might retrofit into the clinical arena. As the newly appointed clinical director of a New Zealand residential program, I contacted Mark Friedman; we agreed to work together.
Structural Family Therapy was the model I had been trained on, based on systems theory, and it guided me through the years. I added the “homeostatic maintainer” component and the essentiality of an organized system of care. I audited my years of treatment of eating disordered patients and published the outcomes in Enduring Change in Eating Disorders: Interventions with Long Term Results (Fishman, 2004). This modified model, Intensive Structural Therapy (IST), was effective.
Mark and I shared a ‘systems thinking’ perspective with an eye to measurably improving services. We set about developing a protocol that would enhance the treatment and allow the team to easily track outcome data. This IST-RBA approach acknowledged the complexity of impoverished families and the treatment would begin with convening all of the stakeholders. In some situations, that could mean 15-20 representative members of non-profit organizations, governmental agencies and the young person’s social network and family. Defining the goals and reaching consensus organizes the de facto community.
Structural Family Therapy was destined to be the great liberator—it did not happen.
The IST-RBA Clinical Scorecard, with fidelity to RBA principles, is the performance measurement tool we introduced. It documents plans and objectives with a focus on targets and measurements that have been developed by all members of the team.
Stevie, age 13, was admitted to our residential program. His father had assaulted him in the school yard. His parents were divorced and in continual conflict. His family had reported more than 33 episodes of family violence to the police over the previous eight years. Stevie was one of four siblings ranging in age from eight to fifteen. He and his 11-year-old brother had been in several out-of-home placements. The large number of behavior problems included expulsions from school, charges for car theft and burglaries, and vandalism in the community, especially the school.
EXAMPLE: Clinical Scorecard for Stevie
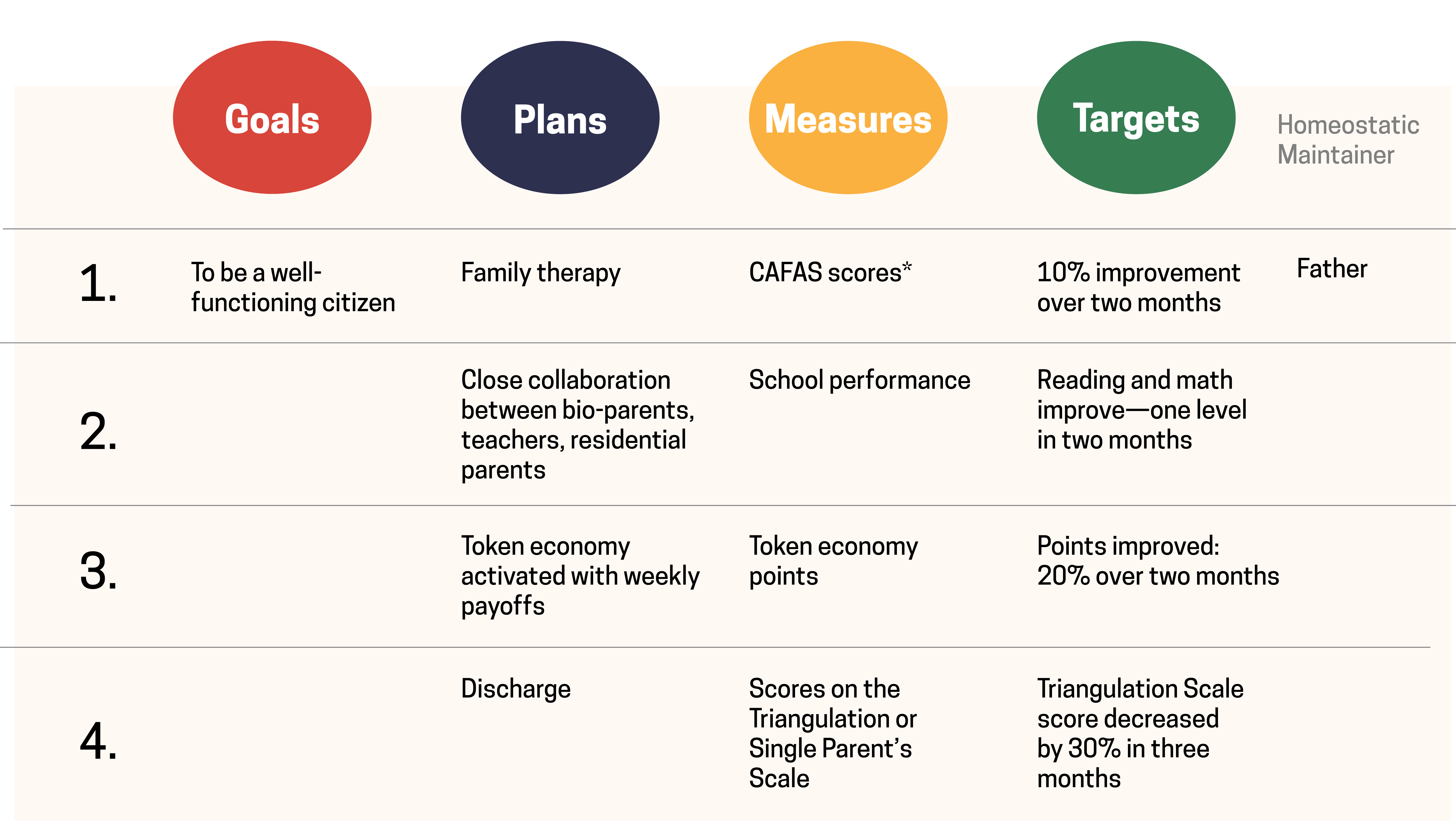
*The Child and Family Functioning Scale (CAFAS) measures 8 domains of a young person’s functioning (Hodges & Kim, 2000).
All stakeholders are identified early on with new members emerging over time. Not one stakeholder can be left out of the Plans for the young person. They determine the Goals and initiate the IST-RBA Clinical Scorecard.
- Build: an organized system of care with stakeholders
- Goals: start with the desired end result and work backwards, in the practice of RBA
- Measures: measure what matters!
- Plans: help the client reach the agreed upon objectives
- Targets: best estimates of measures over a specific time period
- (Reaching a target is used as an intermediate outcome)
- Homeostatic Maintainer: identify those in the therapeutic system who are resisting change
Turning the curve: Tracking performance over time
The slope of the curve determines the outcome of the treatments, while it provides a snapshot letting the team know if the goals are being met. You systematically collect data, track progress, and document by using the Turning the Curve tool.
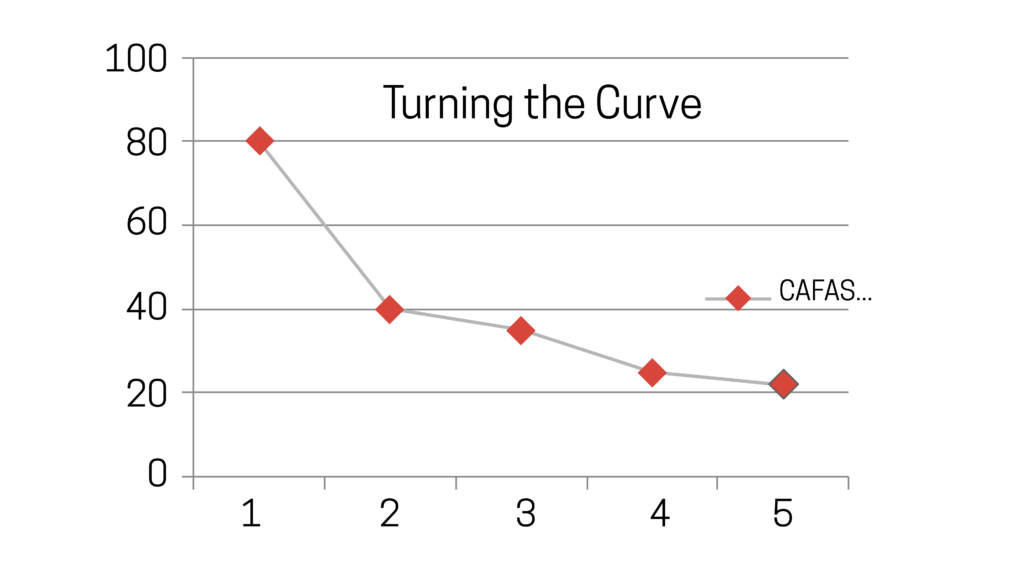
Figure 1: Average CAFAS scores over 5 school terms. (Lower is better)
The benefits of this IST-RBA model include collaborative goal-setting, individualized measures, the transparency of the Clinical Scorecard, and the addition of the Homeostatic Maintainer. The Turning the Curve tool is the graphic evidence of performance. Together, these components help to ensure that all members of the team are clear about the treatment and that interventions are targeted to achieving the desired outcomes.
My cherished time in the halcyon days in Philly had a limitation: the outcomes achieved under supervision were not collected, analyzed and/or published. J. W. Lichtenberg (2007) noted the reason for providing supervision and the ethical justification for requiring it, are that it makes a difference with respect to client outcomes. It would be some years, after Philadelphia, that the scientific world would introduce evidence-based care and that movement did not lumber along the supervisory highway. According to C. Edward Watkins, after reviewing supervision-patient outcome studies for the past 30 years, “we do not seem to be any more able to say now that psychotherapy supervision contributes to patient outcomes” (Watkins, 2011, p. 235). He went on to explain the concept of competent practice and evidence-based practice are more central considerations and psychotherapy supervision now finds itself called to account.
It is my hope that the supervisor encourages the adoption of the Clinical Scorecard and the Turning the Curve tool, with the imperative that the supervisee track outcomes for every patient. Memorializng these outcomes would go a long way to improving care. When using this process, the clinician can become a Local Clinical Scientist, a term coined by George Stricker (2006). For these outcome data to be published and accepted in scientific journals, there must be change in the definition of acceptable data.
Lisbeth B. Schorr, Harvard lecturer and Senior Fellow at the Centre for Social Policy, together with her colleague Frank Farrow, shared the conviction that there should be expansion of the jurisdiction of acceptable data. In their paper, Expanding the Evidence Universe: Doing Better By Knowing More (Schorr & Farrow, 2011; Schorr, 2016), they advise that credible evidence is the agreement of the value of many kinds of interventions that can be assessed, weighed, understood, and acted upon without having to be proven with experimental methods. We clinicians, working at the coalface of families and communities, have much to contribute.
With this enlarged and balanced jurisdiction, all outcomes can be contributed to the global bank. RBA may serve as the search light to liberate those robust hidden data sets so that the mental health field will no longer need to apologize for the waiting list embarrassment. All family therapists become scientists and supervision becomes more accountable and effective. Surely, we can return family therapy to its rightful place as the gold standard treatment to mitigate suffering in families long into the 21st century. The IST-RBA model provides this straightforward methodology to determine whether anybody is better off. Let’s move the needle—go beyond process and let your outcomes shine the light.

H. Charles Fishman, MD, is an AAMFT Professional Member and clinical professor of psychiatry, University of Hawaii, John A. Burns School of Medicine. This article is based on the recently published book, Performance-Based Family Therapy: A Therapist’s Guide to Measurable Change (Fishman, 2022). Fishman Report https://fishman.co.nz email: Charles@fishman.co.nz
REFERENCES
Clear Impact. (2016). What is results-based accountability? Rockville, MD: Author.
Fishman, H. C. (2004). Performance-based family therapy: A therapist’s guide to measurable change. Brunner-Routledge.
Fishman, H. C. (2022). Performance-based family therapy: A therapist’s guide to measurable change. Routledge.
Fraenkel, P. (2022), Whatever happened to family therapy? Psychotherapy Networker, January/February, 23.
Freedman, D. (2009, November). Brave thinkers. The Atlantic. https://www.theatlantic.com/magazine/archive/2009/11/brave-thinkers/307691/
Friedman, M. (2015). Trying hard is not good enough. Santa Fe, NM: Parse Publishing.
Hodges, K., & Kim, C. (2000). Psychometric study of the child and adolescent functional assessment scale: Prediction of contact with the law and poor school attendance. Journal of Abnormal Child Psychology, 28, 287-297. https://doi.org/10.1023/A:1005100521818
Imber-Black, E. (2014). Eschewing certainties: The creation of family therapists in the 21st century. Family Process, 53(3), 371-379. https://doi.org/10.1111/famp.12091
Ioannidis, J. P. (2005). Why most published research findings are false. PLoS Medicine, 2(8), e124. https://doi.org/10.1371/journal.pmed.0020124
Le Grange, D., & Lock, J. (2005). Family-based treatment of adolescent anorexia nervosa: The Maudsley approach. http://www.maudsleyparents.org
Leichsenring, F., Steinert, C., & Ioannidis, J. P. (2019). Toward a paradigm shift in treatment and research of mental disorders. Psychological Medicine, 1-7. https://doi.org/10.1017/S0033291719002265
Lichtenberg, J. W. (2007). What makes for effective supervision? In search of clinical outcomes. Professional Psychology: Research and Practice, 38, 27-28.
Rogers, A. (2017, November 5). Star neuroscientist Tom Insel leaves the Google-spawned Verily for … a startup? Wired. https://www.wired.com/2017/05/star-neuroscientist-tom-insel-leaves-google-spawned-verily-startup/
Schorr, L. B. (2016, January 8). Reconsidering evidence: What it means and how we use it. Stanford Social Innovation Review. https://ssir.org/articles/entry/reconsidering_evidence_what_it_means_and_how_we_use_it
Schorr, L. B., & Farrow, F. (2011, July). Expanding the evidence universe: Doing better by knowing more. Center for the Study of Social Policy. pathways.nccp.org/assets/pdf/SchorrFarrow2011.pdf
Stricker, G. (2006). The local clinical scientist, evidence-based practice, and personality assessment. Journal of Personality Assessment, 86(1), 4-9. https://doi.org/10.1207/s15327752jpa8601_02
Watkins, C. E., Jr. (2011). Does psychotherapy supervision contribute to patient outcomes? Considering thirty years of research. The Clinical Supervisor, 30(2), 235-256. https://doi.org/10.1080/07325223.2011.619417
Other articles
Contextual Family Therapy with Incarcerated Families
Ten million children have experienced parental incarceration (National Resource Center on Children & Families of the Incarcerated, 2009). Incarceration can disrupt entire family systems, affecting psychological, physical, emotional, and financial well-being (Kitzmiller, Cavanagh, Frick, Steinberg, & Cauffman, 2020; Tadros, Fye, & Ray, 2020).
Eman Tadros, PhD and Antonia Guajardo
STUDENT CORNER: Just Another Reason to be Grateful for my Mask
Every clinical hour I’ve obtained so far as a student marriage and family therapist has been through masks or computer screens. I have been accruing hours since September of 2021, and I had my first in-person session at the end of November.
Andrea Kaplan
From Mumbai and Virginia Tech to Houston & Haryana: A Global Journey in Family Therapy Education, Training and Practice
I (MP) was born and raised in the small town of Odisha, and was first introduced to family therapy in a post graduate diploma course in Counseling Psychology in Mumbai, a metropolitan city of India.
Manjushree Palit, PhD and Laurie L. Charlés, PhD



