Working with families living with a disability can often feel overwhelming for beginning and seasoned clinicians. Because there are minimal studies assessing the effectiveness of systemic models and interventions for families living with a disability (Chengappa, McNeil, Norman, Questsche, & Travers, 2017; Llyod & Dallos, 2006; Turns, Jordan, Callahan, Whiting, & Springer, 2019), clinicians often struggle with “saying the right thing,” “using the best intervention,” and “feeling competent to work with families” (despite their systemic training). This article provides clinicians with five easily adaptable interventions for treating a family living with a physical, intellectual, or developmental disability.
1. Coping questions
Families with any kind of disability can face numerous life-long challenges impacting parents, siblings, spouses, and individuals with a disability. Coping questions are designed to help clients identify times and ways they are surviving their pain, loneliness, and fear (De Jong & Berg, 2013). Coping questions can include, but are not limited to: “What have you found helpful so far?”; “How have you managed to cope for so long?”; “How come things are not worse?”; and “How do you manage to get through each day?” (De Jong & Berg, 2013).
Throughout treatment, it can be beneficial to ask coping questions as a way to identify how the client has done so well given their challenging circumstances. While treating mothers raising a child with a developmental disability, most break down and cry when asked, “How have you managed to cope with all of these challenges and stressors?” Parents typically respond by stating, “No one has ever asked us that. We don’t think anyone sees how hard we’re trying. [Professionals] just give us more to do and explain everything we aren’t doing right.”
 This intervention is specifically useful when helping parents or spouses process a recent diagnosis and prognosis. While working with a client, her husband suffered an accident, leaving him paralyzed from the waist down and unable to control his bladder and bowel movements. Many sessions were spent helping the client identify how she was coping with the diagnosis. Additionally, she discussed coping with becoming a full-time nurse and helping her husband use the restroom.
This intervention is specifically useful when helping parents or spouses process a recent diagnosis and prognosis. While working with a client, her husband suffered an accident, leaving him paralyzed from the waist down and unable to control his bladder and bowel movements. Many sessions were spent helping the client identify how she was coping with the diagnosis. Additionally, she discussed coping with becoming a full-time nurse and helping her husband use the restroom.
The miracle question
One of the most common mistakes clinicians make when working with a family or individual with a disability is assuming the clients are seeking therapy because of the diagnosis. Although many of the presenting problems and challenges are related to a diagnosis, therapists should not assume families are seeking treatment due to the diagnosis. After assessing a family’s goals for treatment, the miracle question can help families identify small, immediate changes they would notice in their lives if the presenting problem (i.e. behaviors and challenges, not the disability) no longer existed:
“Suppose a miracle happened tonight, while you were sleeping, causing all of the problems that brought you to therapy, to disappear. What would be different that would tell you the miracle happened and the problem that brought you here was solved?” (adapted from de Shazer, 1988, p.5)
Rather than thinking all problems must be solved at once, the miracle question allows clients to think about their ideal day; specifically, what behavioral changes would they make if their problem were gone. It’s important to note, answers should be realistic. A disclaimer could be used such as, “Unfortunately, we cannot change your child’s diagnosis, but how would his lack of outbursts alter your miracle day?”
While assessing the effectiveness of solution-focused brief therapy (SFBT) for couples raising a child with autism, Turns and colleagues (2019) discovered mothers’ distaste for the Miracle Question (MQ). All five mothers believed the MQ was confusing and felt vulnerable. Statements such as, “I’m not sure I understood what [the therapist] was asking for” and “I’ve closed [possible miracles] so I wouldn’t be hurt anymore…” (Turns, Olufowote, Jordan, & Chavez, in press, p.18). Due to these reflections and the insensitivity the term “miracle” may have on a family living with a life-long disability, we recommend stating “shift” or “jolt,” rather than the term miracle.
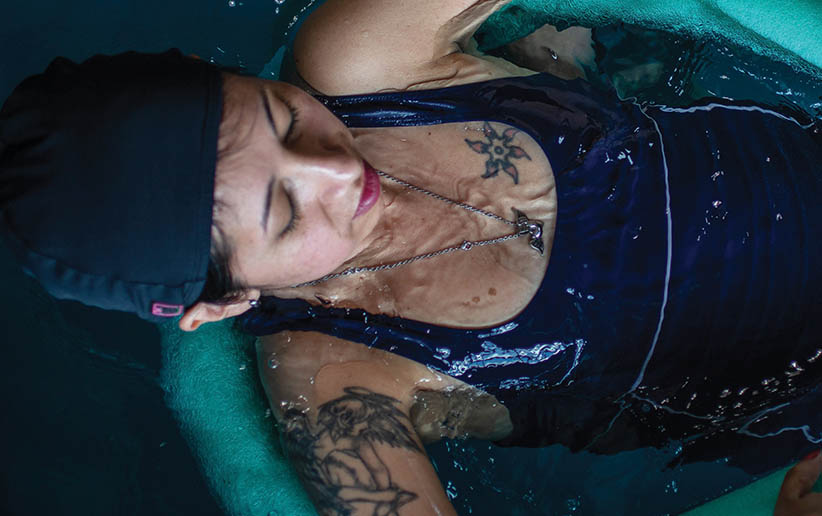
 Calm / Safe Place exercise
Calm / Safe Place exercise
Many children and adults who have a disability may have experienced a trauma (Tsakanikos et al., 2007). The Safe/Calm Place exercise is a standard exercise when working with individuals who have experienced trauma (Shapiro, 2018). The goal of this exercise is to create a place where clients can self-soothe when they do not feel safe or calm and stay emotionally-regulated (Shapiro, 2018). This intervention is typically used to end a session or as a way clients can deal with disturbing material between sessions.

Setting up a Safe Place has several steps. First, the clinician and the client can identify an image or safe place that creates a personal feeling of calm and safety. Oftentimes, adult clients with a disability may choose a place outdoors (e.g., lake, beach, mountains), while children may choose fantasy places (e.g., Hogwarts). Next, therapists help the client develop bodily sensations with the image. Asking questions such as, “As you think of that place, what do you see, smell, hear?” can enhance the visualization and make it a more inviting and safer place. Third is to further enhance the imagery by creating additional details; for example, ask questions such as “How warm/cold is it there?” “What does the breeze feel like?” In the fourth step, have the client “sit” in the place and make sure it is completely safe and pleasant for them. If during this step, the client finds something disturbing, the client can create a new place. Taking time in session to practice this exercise will help the client develop skills to self-soothe when distressed.
Sandtray
 Sandtray therapy allows clients of any age to visually demonstrate internal experiences, including thoughts, emotions, ideas, strengths, and frustrations, with figures or miniatures (Isom, Groves-Radomski, & McConaha, 2015). Clients are provided with vague instructions, such as, “I would like you to create your world in the sandtray. While looking at the figurines on the shelves, select anything you would like to be represented in your world. The only rule is your world cannot be based on a movie or video game.”
Sandtray therapy allows clients of any age to visually demonstrate internal experiences, including thoughts, emotions, ideas, strengths, and frustrations, with figures or miniatures (Isom, Groves-Radomski, & McConaha, 2015). Clients are provided with vague instructions, such as, “I would like you to create your world in the sandtray. While looking at the figurines on the shelves, select anything you would like to be represented in your world. The only rule is your world cannot be based on a movie or video game.”
When working with siblings of an individual with a disability, sandtray therapy can provide a creative outlet to show their world and experiences. Siblings often report feeling ignored or believing their parents spend more time with their sibling than them. Sandtray therapy provides a non-confrontational way for clients to express their experiences.
When processing a client’s tray, therapists are advised to sit close to display respect and interest in their tray. Therapists should never touch an item in a client’s tray or name the figures (Homeyer & Sweeney, 2011). It is vital for therapists to “keep the discussion within the metaphor or story of the tray” (Homeyer & Sweeney, 2011, p. 45). For example, “You told me this dragon is really scary. Tell me more about that.” If a client breaks the metaphor such as, “This is my brother,” the therapist should proceed with caution.
Although this activity can be used with the entire family and with individuals with a disability, siblings of those with a disability can provide a wealth of information. For example, when working with a teenage girl who had two older siblings with autism, I (B.T.) asked her to create her world in the tray. After 12 minutes of staring at the shelves and back into the empty tray, she stated she “didn’t have a world.” This information contributed to understanding the family system and why her presenting problem may have existed. Another sibling, with a younger sister with Downs, portrayed a world where a knight was protecting a princess on her horse. In a later session, more information was shared about the sibling’s role of protecting the sister in public and with peers at school.
 Relationship check-in
Relationship check-in
When working with families with a disability, it is critical to take time to assess the martial/couple relationship. Parenting is one of the most challenging things a couple will do together, and when one adds a child with a disability in the system, it can shock even the strongest marital relationship.
When couples first discover their child has a disability, they often grapple with feelings of guilt, grief and anger. They may wonder if they could have done “something” sooner, and unfortunately many couples often blame themselves (and each other) for their child’s struggles and behaviors. This is magnified if professional experts (i.e. doctors, school counselors, teachers, therapists) are questioning them about their parenting skills. This often leads to a negative internalization cycle, furthering anxiety and stress.
The consequences of the relationship strain can be serious, not only for the individual with a disability, but the entire family. Marital stress is associated with serious physical health problems, as well as symptoms of depression and other mental health problems (McShall & Johnson, 2015). The child with a disability is often the casualty of this stress, and can manifest additional behavioral symptoms associated with problems in the marriage. In an attempt to deal with the shame and frustration, the couple will often further isolate themselves from friends and peers. They also may develop a pattern where one spouse spends more time at work (as a means to cope), while the other experiences an increasing percentage of the child care.
A family system is only as healthy as the couple relationship. Taking time to assess the couple’s relationship is critical, even if the couple is originally coming for help in parenting their child with a disability. Doing basic relationship check-ins can give the couple an opportunity to assess where their relationship is at, and to give it the necessary attention it needs. Creating a safe and secure avenue for couples to honestly communicate with one another creates opportunities for connection as they are able to name what they are feeling and develop goals to reconnect with one another. When doing relationship check-ins, it is critical to assess the following: 1) their level of intimacy, 2) communication patterns, 3) conflict resolution skills, 4) how they honor time for each other, and 5) what shared goals they have together. Ultimately, this simple relationship check-in can serve as a metric in understanding how the couple communicates, and what areas in their relationship need greater enhancement.
Many of the systemic models used by marriage and family therapists can be very beneficial when used with families living with a disability. However, there is a drastic lack of research and published material on the effectiveness and application of these interventions. These five interventions have been widely beneficial for many individuals and families living with a disability.
This article is offered free by AAMFT. If you are interested in accessing other content, join today!

Brie Turns, PhD, LMFT, is an AAMFT Clinical Fellow and AAMFT Approved Supervisor and an assistant professor in the Marriage and Family Therapy Department at Fuller Seminary Arizona. Her research and clinical specialization is families raising a child with autism. She has published numerous publications and presented at international and national conferences regarding families and ASD. Turns recently co-edited Systemically Treating Autism.

Paul Springer, PhD, LMFT, is an AAMFT Clinical Fellow and AAMFT Approved Supervisor, a full professor in the Marriage and Family Therapy Program at the University of Nebraska-Lincoln, as well as the Associate Dean for Student Success in the College of Education and Human Sciences. His research interests include access to mental healthcare services for vulnerable and underserved populations in rural and global communities. Springer has actively presented his work in multiple countries throughout the world, including Jordan, Spain, Portugal, England, Brazil and China.
REFERENCES
Chengappa, K., McNeil, C. B., Norman, M., Questsche, L., B., & Travers, R. M. (2017) Efficacy of parent-child interaction therapy with parents with intellectual disability. Child and Family Behavior Therapy 39(4), 253-282.
De Jong, P. & Berg, I. K. (2013). Interviewing for solutions (4th ed.). Brooks/Cole
de Shazer, S. (1988). Clues: Investigating solutions in brief therapy. W. W. Norton & Company.
Homeyer, L.E., & Sweeney, D. S. (2011). Sandtray therapy: A practical manual (2nd ed.). Routledge.
Isom, E. E., Groves-Radomski, J., & McConaha, M. M. (2015). Sandtray therapy: A familial approach to healing through imagination. Journal of Creativity in Mental Health, 10(3), 339-350.
Lloyd, H. & Dallos, R. (2006). Solution focused brief therapy with families who have a child with intellectual disabilities: A description of the content of initial session and the processes. Clinical Child Psychology and Psychiatry, 11(3), 367-386.
McShall, J. R., & Johnson, M. D. (2015). The association between relationship distress and psychopathology is consistent across racial and ethnic groups. Journal of Abnormal Psychology, 124(1), 226-231.
Shapiro, F. (2018). Eye movement desensitization and reprocessing (EMDR) therapy: Basic principles, protocols, and procedures (3rd ed.). Guilford.
Tsakanikos, E., Bouras, N., Costello, H., & Holt, G. (2007). Multiple exposure to life events and clinical psychopathology in adults with intellectual disability. Social Psychiatry and Psychiatric Epidemiology, 42, 24-28.
Turns, B., Jordan, S. S., Callahan, K., Whiting, J., & Springer, N. (2019). Assessing the effectiveness of solution-focused brief therapy for couples raising a child with autism: A pilot clinical outcome study. Journal of Couple & Relationship Therapy, 18(3), 257-279.
Turns, B., Olufowote, R. D., Jordan, S. S., & Chavez, M. S. (in press). When the therapist described our strengths, I kind of saw a light at the end of the tunnel”: Experiences of solution-focused brief therapy for couples raising a child with ASD. The Qualitative Report.
Other articles
Disability and Stigma
Disability is often perceived by society as a negative experience and something unwanted. As systemic therapists, we are accountable for our stigmas and biases towards disabled clients and their families.
Briana Mills, MSMFT
Neurodivergent Identity Formation: Are We Listening?
Marriage and family therapists are uniquely equipped to offer therapy that not only nurtures the personal identity exploration journey of neurodivergent clients, but also the interpersonal dynamics surrounding the process.
Kelli Willard, MA
Disabilities and the Family: Where are the Marriage, Couple, and Family Therapists?
Systemic therapists have an opportunity to play a key role in bridging the gap to address the growing need for accessible mental health services that support individuals with disabilities and their families by managing risks and enhancing resilience.
M. L. Parker, PhD and Kami L. Gallus, PhD